March 30, 2021
The California Department of Health Care Services (DHCS) recently released the Preventive Services Report, a first-ever report (plus an Addendum) detailing how different populations of children and youth are accessing preventive care in Medi-Cal. The Department used data from calendar year 2019, prior to the COVID-19 pandemic. One of the main findings is that overall, an alarmingly low number of children and youth in Medi-Cal are receiving preventive health care check-ups and screenings.
Children are legally entitled to a variety of preventive and medically necessary services through Medi-Cal. The Early & Periodic Screening, Diagnosis & Treatment benefit applies to all children under the age of 21 and covers preventive care such as well-child visits, dental, vision, hearing and trauma screenings and vaccinations; timely access to and coordination with language-appropriate care; and any treatments a child may need for a physical or mental condition.
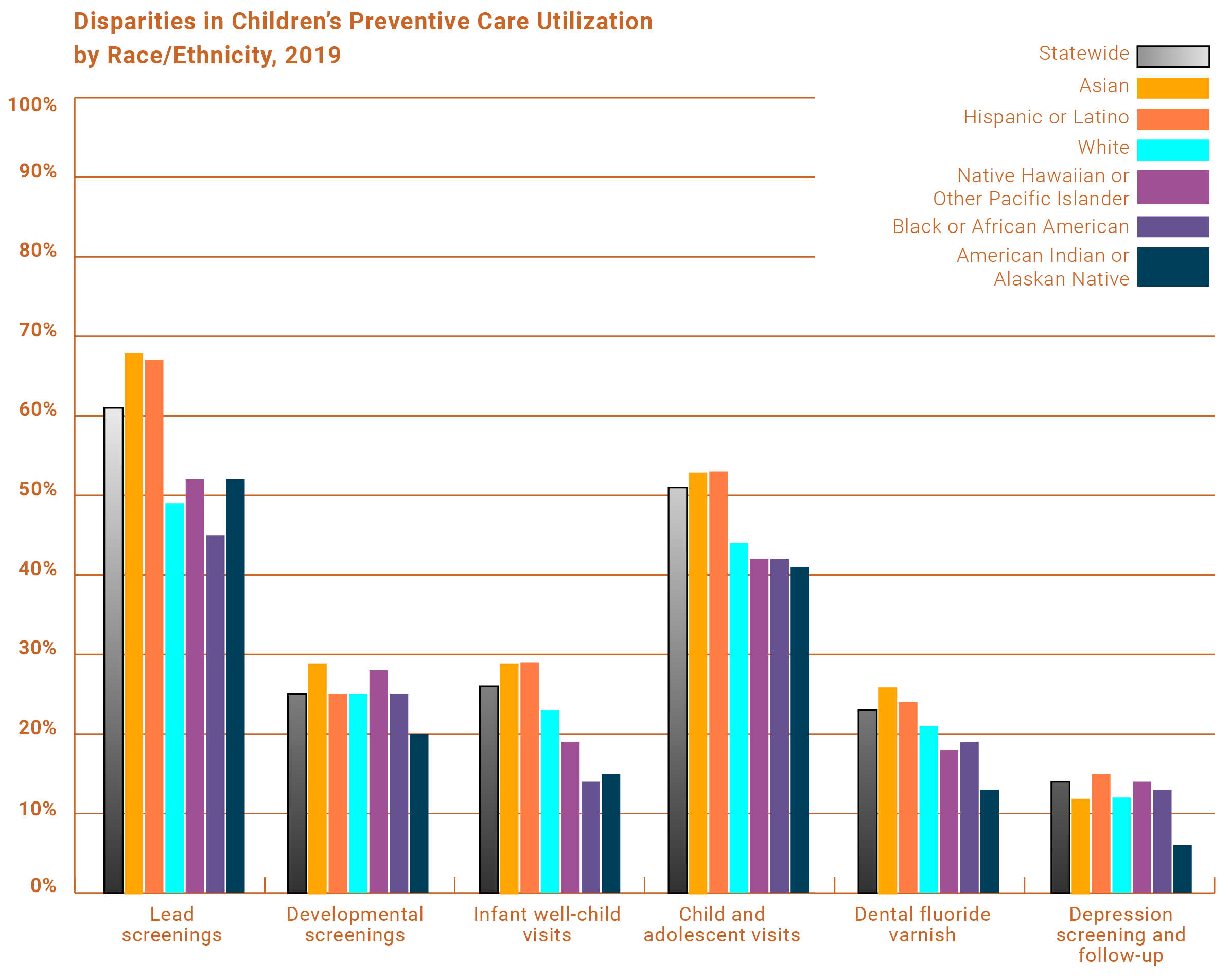
However, according to the report, too many children are not receiving these screenings and check-ups, for example:
- 3 out of 5 young children were screened for elevated blood lead levels.
- 1 out of 4 children were screened for risk of developmental delays.
- 1 in 4 infants had all their pediatrician-recommended well-care visits.
- 1 in 2 children and adolescents had an annual check-up.
- 1 out of 4 children and youth received dental fluoride varnish treatments.
- 1 out of 7 youth who were screened for depression received a follow-up plan.
- 1 out of 50 young adults were screened for alcohol use.
Additionally, the findings add to the growing body of evidence showing troubling racial, ethnic, and language inequities for children’s services in Medi-Cal. Data have consistently shown that Black, American Indian or Alaskan Native, Native Hawaiian or other Pacific Islander, and children living in households that speak a language other than English are even less likely to receive crucial preventive services to which they are entitled.
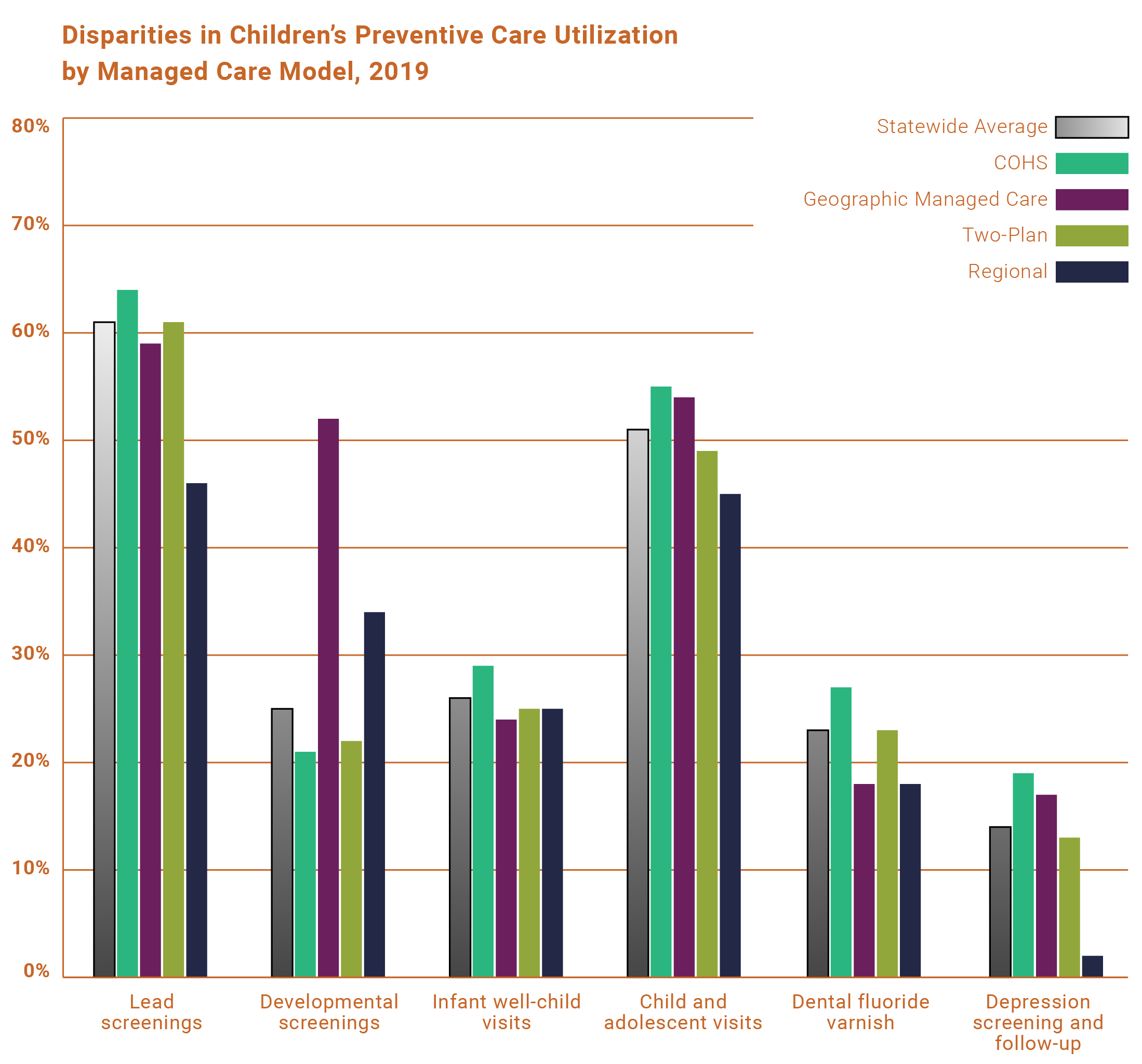
In addition, the Preventive Services Report shows the variation in children’s care based on which county they live in and what Medi-Cal managed care looks like in that county. Rates of services in rural areas of the state were consistently lower than for urban areas – sometimes by just a little, and sometimes by a lot. The type of Medi-Cal managed care model also made a difference. Plans in the County Organized Health Systems (COHS) model of managed care, in which there is only one health plan, generally had higher rates than plans in other types of competitive models.
State leaders must begin to develop and implement comprehensive strategies with multipronged solutions that address the distinct needs of California’s children and take into account the state’s racial/ethnic, linguistic, and geographic diversity. Specifically, California should take the following steps this year to tackle these systemic equity issues:
- Use accountability to improve quality of care for kids in Medi-Cal. DHCS should ensure its upcoming administrative reform efforts – such as the California Advancing and Innovating Medi-Cal (CalAIM) initiative, efforts to select Medi-Cal managed care plans, and contracting for administration of the Medi-Cal Dental benefit – are focused on health equity and quality improvement for children’s care. The State can dramatically improve the quality of care for kids by ensuring compliance with existing contractual requirements, aligning payments and incentives with measurable outcomes and performance, and proactively eliminating disparities in children’s health outcomes. (Read Children Now’s comments on the CalAIM proposal here.)
- Protect and prevent cuts to children’s health services. State data clearly show that racial/ethnic, linguistic, and geographic disparities existed in children’s preventive care prior to the pandemic, and COVID-19 only made things worse by overloading health care systems. It is imperative that the State take all necessary steps to protect children’s health programs and promote the stability of the Medi-Cal program as California rebounds from the pandemic. This includes maintaining voter-approved payments for doctors to provide kids with check-ups and screen them for trauma and developmental delays – services that are important now more than ever given the devastating and potentially long-term impacts of the pandemic on children’s well-being. (Learn more here about how Proposition 56 funds are a critical support for children’s health in Medi-Cal.)
- Enact Senate Bill 682 (Rubio), which would require the California Health and Human Services Agency to create a plan that intentionally and proactively responds to known racial disparities in the areas of five children’s chronic disease: asthma, diabetes, dental caries, depression, and vaping-related diseases. With a race-centered and equity-focused plan in place that clearly articulates the outcomes for closing racial gaps in childhood chronic disease, the State can truly begin to ensure all of California’s children become healthy adults. (Read the legislative text of SB 682)
