By Health Team
February 23, 2023
Updated August 30, 2023
Top image via iStock from PeopleImages
For over two decades, California has made tremendous progress toward getting all kids connected to health coverage, including a huge win in 2022 to eliminate Medi-Cal premiums for over 500,000 Californians and an expansion of Medi-Cal to include undocumented young adults ages 19-25 which took effect in 2020.
WHY CONTINUOUS HEALTH COVERAGE IS IMPORTANT
We know that kids with continuous health insurance, like Medi-Cal for Kids & Teens, have better health and economic outcomes. Since the onset of the COVID-19 Public Health Emergency in March 2020, important federal provisions have protected Californians from losing their Medi-Cal coverage. As a result, children’s Medi-Cal enrollment has grown by nine percent, and more than 56% of children are now covered by Medi-Cal, according to a new report from the Georgetown University Center for Children and Families. As champions for children’s health, we must work together to ensure all children can access the healthcare services they need.
MEDI-CAL COVERAGE COULD NOW BE AT RISK FOR THE MILLIONS OF KIDS AND FAMILIES WHO RELY ON IT
In April, the federal Medicaid protections officially came to an end and the state and counties are now restarting the renewal process for all 15 million Californians covered by Medi-Cal, including over 5.6 million children. Recent state data show that one in three – that’s almost 70,000 kids and youth – of the more than 225,000 Californians who were disenrolled from Medi-Cal in June were under the age of 21. However, many kids may still be eligible for coverage because the vast majority of disenrollments (89%) were due to procedural reasons. For example, the state and county may have outdated contact information for the family so they cannot reach them, or information was not provided in the family’s primary language or in a manner that is easy for the family to read and understand. High procedural disenrollment rates are concerning because many people who are disenrolled for these paperwork reasons may still be eligible for Medi-Cal coverage and this is particularly concerning when we see that children accounted for 1 in 3 disenrollments in our state.
During the month of August, there are approximately 1 million Californians that need to return their renewal packets. While some children and families may see their Medi-Cal coverage auto-renewed, for some families, this may be the first time they receive and need to complete the Medi-Cal renewal paperwork. Educating and linking families and caregivers to support when needed will help minimize unnecessary disruptions or drops in coverage for kids due to paperwork. For example, parents and caregivers may be unaware of the higher income cut offs in Medi-Cal for children and youth which could cause confusion in a household when other household members lose eligibility for Medi-Cal coverage. Similarly, families who received a disenrollment notice may not be aware that they can still return their renewal information and have their Medi-Cal reinstated back to their original enrollment date—if they act by September 30, 2023.
It’s critical for parents to complete a renewal form even if they don’t think they are eligible, as their child(ren) might be.
WHAT YOU CAN DO TO HELP
We all play a role in helping families navigate the Medi-Cal renewal process by sharing information and reminders, providing individualized support, or connecting families to the network of supports that are available locally. Perhaps you, someone you know, or someone you serve in your community relies on Medi-Cal to stay healthy. Trusted organizations or businesses in your community have the power to help us keep kids covered by letting families with Medi-Cal know the steps they’ll need to take to keep their coverage:
Families Must Complete Their Medi-Cal Renewals
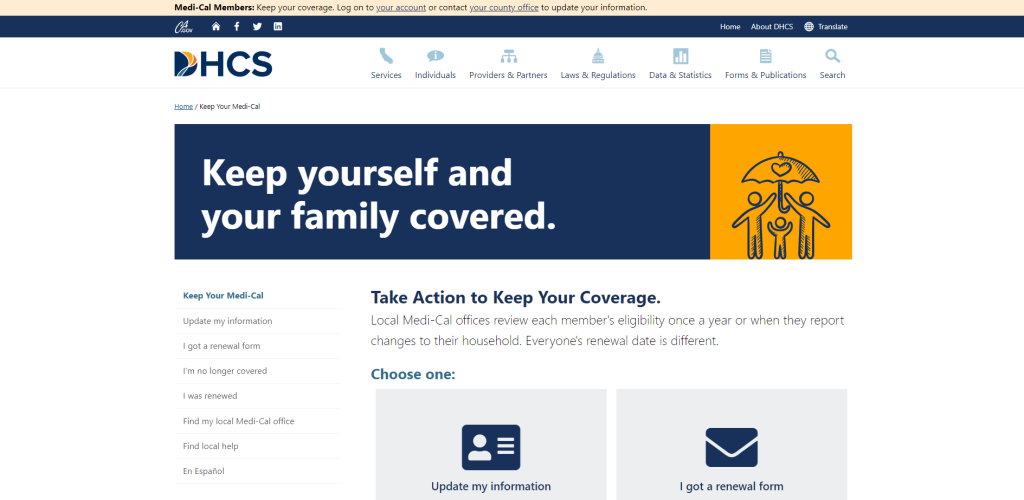
Families can update their contact information to ensure they receive their renewal packet (it will arrive in a yellow envelope) and complete renewals through online portals.
-
Covered California Portal
- Covered California is available statewide. Visit Covered California for more information about how to access your online account or call the service center at (800) 300-1506.
-
BenefitsCal portal
- BenefitsCal is phasing in statewide in 2023. Visit BenefitsCal for more information about how to access your online account.
-
My Benefits CalWIN portal
- My Benefits CalWIN is available in certain counties. Visit My Benefits CalWIN for more information about how to access your online account.
- Update contact information: The state is encouraging beneficiaries to contact their county office by mail, phone, in person, or online to update current contact information (name, mailing address, phone number, email address) and report any changes in family circumstances, such as a new baby.
- Look out for information about renewals: Starting in February 2023, some Medi-Cal members will begin receiving renewal forms in yellow envelopes.
- Respond right away: To avoid a gap in Medi-Cal coverage, members will need to submit any requested information by mail, phone, in person, or online (see box).
Families can visit KeepMediCalCoverage.org to sign up for email and text message alerts with updates about Medi-Cal renewals.
IMPORTANT NOTE TO FAMILIES: There have been reports nationwide of scammers contacting Medicaid members requesting a fee to help apply for or renew Medicaid (Medi-Cal in CA) coverage. Medi-Cal NEVER requires payment during the application or renewal process. If you suspect Medi-Cal fraud, report it here: https://www.dhcs.ca.gov/individuals/Pages/StopMedi-CalFraud.aspx
MORE RESOURCES
Connecting Families to Support When they Need Help. Two great resources to assist families with renewals are:
- Health Consumer Alliance (888-804-3536 or www.healthconsumer.org), which can help families navigate the complexities of renewal, or contest a termination decision that is unwarranted.
- Medi-Cal Health Enrollment Navigators, are community-based organizations and other local organizations that provide enrollment and renewal support to families and caregivers to stay covered. View a list of Navigators broken down by county here.
Educating Families About Medi-Cal Renewals. Two great resources to educate families about Medi-Cal renewals and what to do are:
- Medi-Cal Continuous Coverage Unwinding and Redeterminations Outreach Materials and Resources: As part of its effort to keep kids covered, the state has created a number of resources in the 19 Medi-Cal threshold languages for stakeholders, including messages and flyers, that can be shared widely at community centers, Women, Infants, and Children (WIC) and CalFresh offices, hospitals, clinics, pharmacies, school nurse offices, school health centers, local county offices, afterschool programs, parent organizations, child care centers, and any other organizations working directly with Medi-Cal beneficiaries. Family Voices of California created a series of educational videos in English and Spanish and one-page guides to provide clear, concise, and family-friendly information about Medi-Cal renewal.
Additional Support for Health Coverage Enrollers, Navigators, CBOs, etc.: The Children’s Partnership (TCP) & the National Health Law Program (NHeLP) are hosting a series of Medi-Cal renewal feedback loops to identify and address issues and concerns with the Medi-Cal renewal process. If you are a community-based organization, health care navigator, enrollment assister, community health worker/promotora, provider, or other stakeholder, register to attend these timely and informative discussions the third Wednesday of the month at 12 pm PST. Interpretation services will be provided upon request. Register here.
This blog post will be updated with new resources/materials as they become available.